Two Lenses, One Struggle:
Comparing TCM and Western Approaches to Anxiety
As anxiety and mood disorders become more widely acknowledged in mainstream health care, the search for effective treatment continues to grow. In Western medicine, these conditions are typically diagnosed based on symptom clusters—generalized anxiety disorder, panic disorder, depression, and others—defined in clinical manuals like the DSM-5. Treatments often rely on pharmaceutical intervention, including SSRIs, benzodiazepines, and beta blockers, along with cognitive behavioral therapy (CBT) and other forms of counseling. These approaches aim to reduce or manage symptoms, and for many people, they provide critical relief.
Western Medicine vs. TCM –
Approaches to Anxiety
| Aspect | Western Medicine | Traditional Chinese Medicine (TCM) |
|---|---|---|
| Diagnosis | Based on symptoms and standardized categories (e.g., GAD, depression) | Based on underlying pattern of disharmony (e.g., Heart yin deficiency, Liver qi stagnation) |
| Focus of Treatment | Symptom management through medication and therapy | Restoring internal balance and treating root cause |
| Primary Tools | Pharmaceuticals, psychotherapy, behavioral interventions | Herbal medicine, acupuncture, qigong, dietary and lifestyle changes |
| View of Emotions | Mental or neurological dysfunction | Expression of organ and energetic imbalance |
| Time Frame | Often rapid symptom relief, long-term medication use common | Gradual regulation and long-term systemic improvement |
| Side Effects | Medication side effects (e.g., drowsiness, dependency) | Fewer if properly prescribed; mild digestive effects possible |
| Integration Potential | Common in conventional settings; increasingly open to mindfulness techniques | Can complement Western care, especially in chronic or stress-related cases |
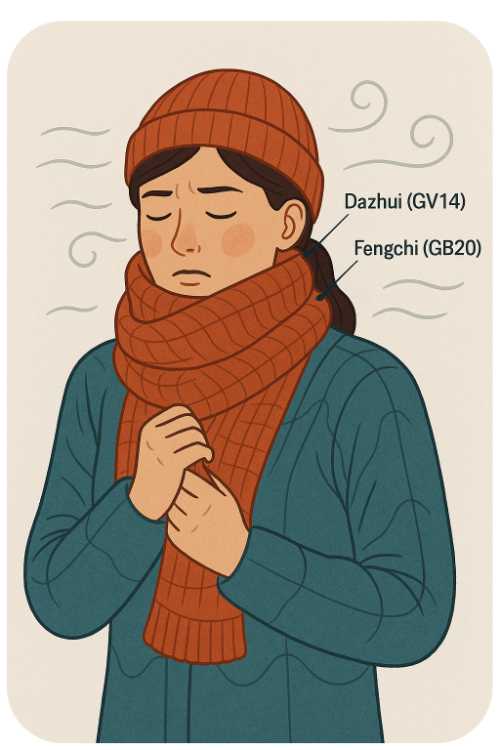
But Traditional Chinese Medicine (TCM) views anxiety through a very different lens. Rather than focusing on the brain as the source of mental illness, TCM sees emotional disturbances as systemic imbalances—patterns involving the Heart, Liver, Spleen, and Kidney systems, and disruptions in the flow of Qi and blood. Anxiety is not considered a disease category on its own, but a manifestation of deeper disharmony. This allows treatment to be individualized, even among patients with similar symptoms.
For example, two people might both be diagnosed with anxiety in Western medicine, but receive completely different treatments in TCM. One may have Heart Yin deficiency—leading to insomnia, palpitations, and overthinking. Another might have Liver Qi stagnation, with chest tightness, irritability, and digestive issues. Instead of prescribing the same medication, a TCM practitioner would select different acupuncture points, herbal formulas, and lifestyle guidance based on these underlying patterns.
This contrast in diagnostic approach also affects how each system views treatment goals. Western medicine often aims to regulate neurotransmitters and stabilize mood. TCM seeks to restore internal balance, nourish deficient organs, and promote the smooth circulation of energy. In that sense, Western methods may offer more immediate symptom control, while TCM focuses on long-term regulation and prevention.
Another key difference is the understanding of side effects. In Western medicine, medications can sometimes cause drowsiness, dependency, or digestive upset. In TCM, formulas are composed of multiple herbs that work in concert, designed to balance one another and minimize adverse reactions. Even so, herbal treatments are not risk-free and require proper diagnosis and oversight.
Interestingly, both systems increasingly find common ground. Practices like acupuncture and qigong are now supported by research showing reductions in cortisol levels and improvements in mood and sleep. Mindfulness-based therapies, which share roots with Daoist and Buddhist thought, are used in Western clinics. The boundaries are beginning to blur, and patients often benefit from an integrative approach.
Ultimately, the question is not which system is “better,” but how they can complement one another. A person taking medication might use acupressure or herbal teas to support sleep. Someone practicing qigong may still benefit from counseling. By viewing anxiety not just as a disorder to suppress, but as a signal of imbalance to explore, TCM offers a gentle but profound pathway back to emotional health.
Vocabulary Guide
- Qi (气): Vital energy flowing through the body, central to all TCM theory
- Heart yin deficiency: A pattern involving depletion of nourishing fluids, often linked to insomnia and anxiety
- Liver qi stagnation: A common TCM pattern related to stress, frustration, and emotional suppression
- DSM-5: Diagnostic and Statistical Manual of Mental Disorders, used in Western psychiatry
- SSRIs: Selective serotonin reuptake inhibitors, a class of antidepressants
- Acupuncture: Use of thin needles at specific points to regulate energy and organ function
- Qigong (气功): Gentle movements and breathwork used to cultivate and balance internal energy